A firm diagnosis of malignant mesothelioma needs to be made before an effective treatment plan can be put into place, and after that initial diagnosis is made surgeons need to be able to distinguish between benign and malignant tissue. Prior to surgery they rely on biomarkers to guide them, but several of these markers exist and some are more accurate than others. A new study from Canadian pathologists is aimed at providing guidance for these physicians as they move forward.
Guidance on Selection of Mesothelioma Markers Published in Pathology Journal
The new guidance on selecting markers for malignant mesothelioma comes from Andrew Churg, MD, of the Department of Pathology at the University of British Columbia, in Vancouver, British Columbia, Canada and his co-author, Julia R. Naso, MD, PhD. Speaking of the article, which appeared in The American Journal of Surgical Pathology, Dr. Churg explained that choosing the right biomarker requires an understanding of different tumor types and of which types of tumors are more likely to appear in different locations.
Dr. Churg said, “Separating benign mesothelioma reactions from malignant mesotheliomas is crucial to patient care and prognosis, since most pleural malignant mesotheliomas are highly aggressive tumors with limited treatment options and a dismal prognosis. Many peritoneal mesotheliomas fare better but require very specialized therapy—cytoreductive surgery and [heated] intraperitoneal chemotherapy.”
Benign and Malignant Mesothelioma Cells Can Mimic Each Other
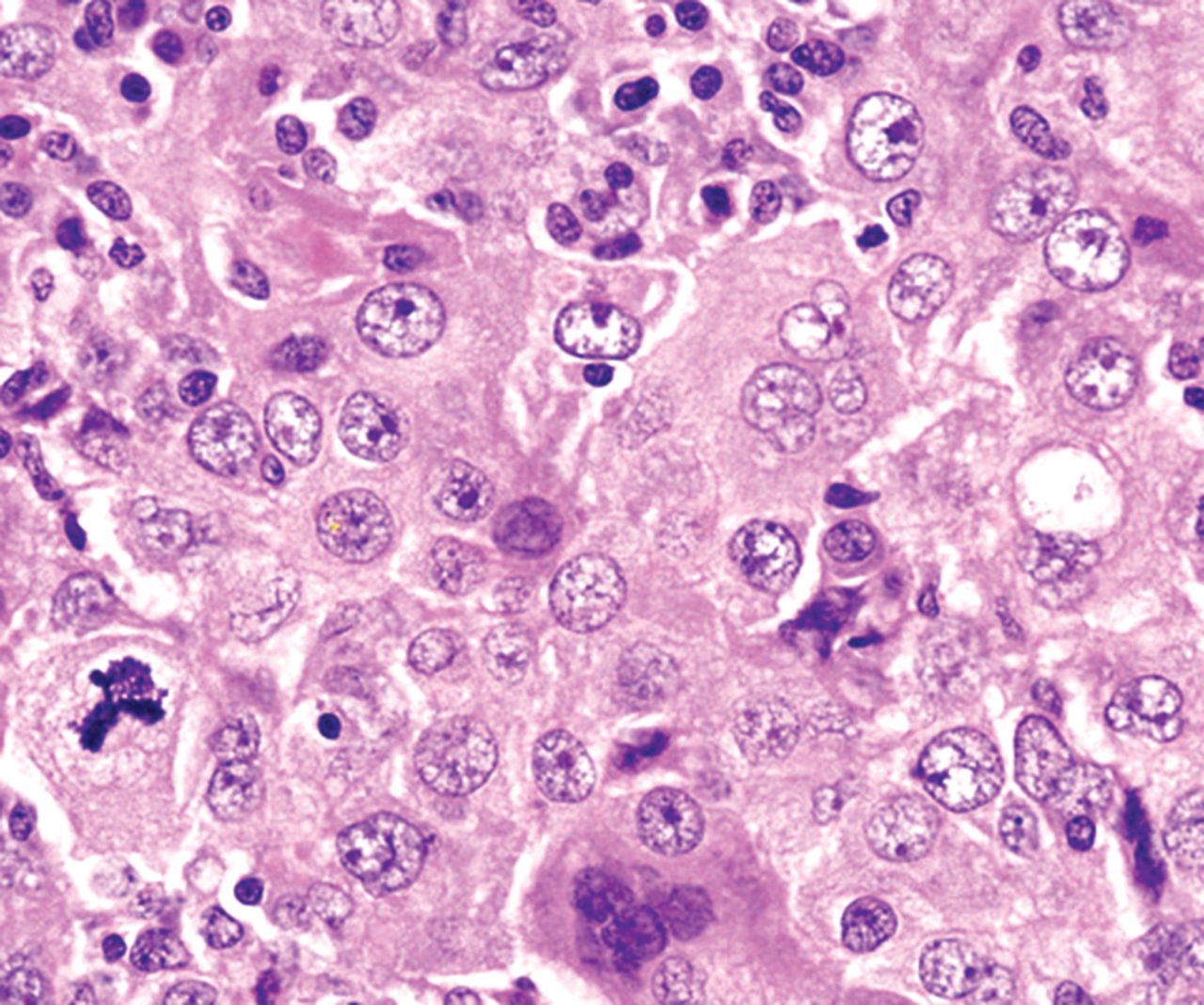
Dr. Churg explained that mesothelioma proliferations can look alike, even though some may be benign and others malignant. Newer approaches to identifying and distinguishing between them rely upon detecting known genetic abnormalities through the careful selection of biomarkers. Both morphology and body cavity seem to affect marker sensitivity, and the pathologists have found that many of the markers that have been used over the last two decades have not been specific enough: they may be useful for general assessments of patient groups, but not for individuals.
In summarizing their findings, Drs. Churg and Naso suggest a morphology- and location-based approach to selection of a marker test for individual patients, and write, “At this point there are 3 well established adjunctive markers for separating benign from malignant mesothelial proliferations, BAP1 IHC, MTAP IHC, and CDKN2A FISH, and we suggest that these should be the first approach to the problem, with consideration given to the morphology (epithelial vs. spindle) and location (pleura vs. peritoneum). The other markers described in this review either have inconsistent published results (NF2 FISH) or simply too few publications to recommend them.”
If you or someone you love has been diagnosed with malignant mesothelioma, this latest information can guide your surgeon’s decisions regarding your care. For more helpful resources, contact the Patient Advocates at Mesothelioma.net at 1-800-692-8608.
